Understanding Digestive System Disorders
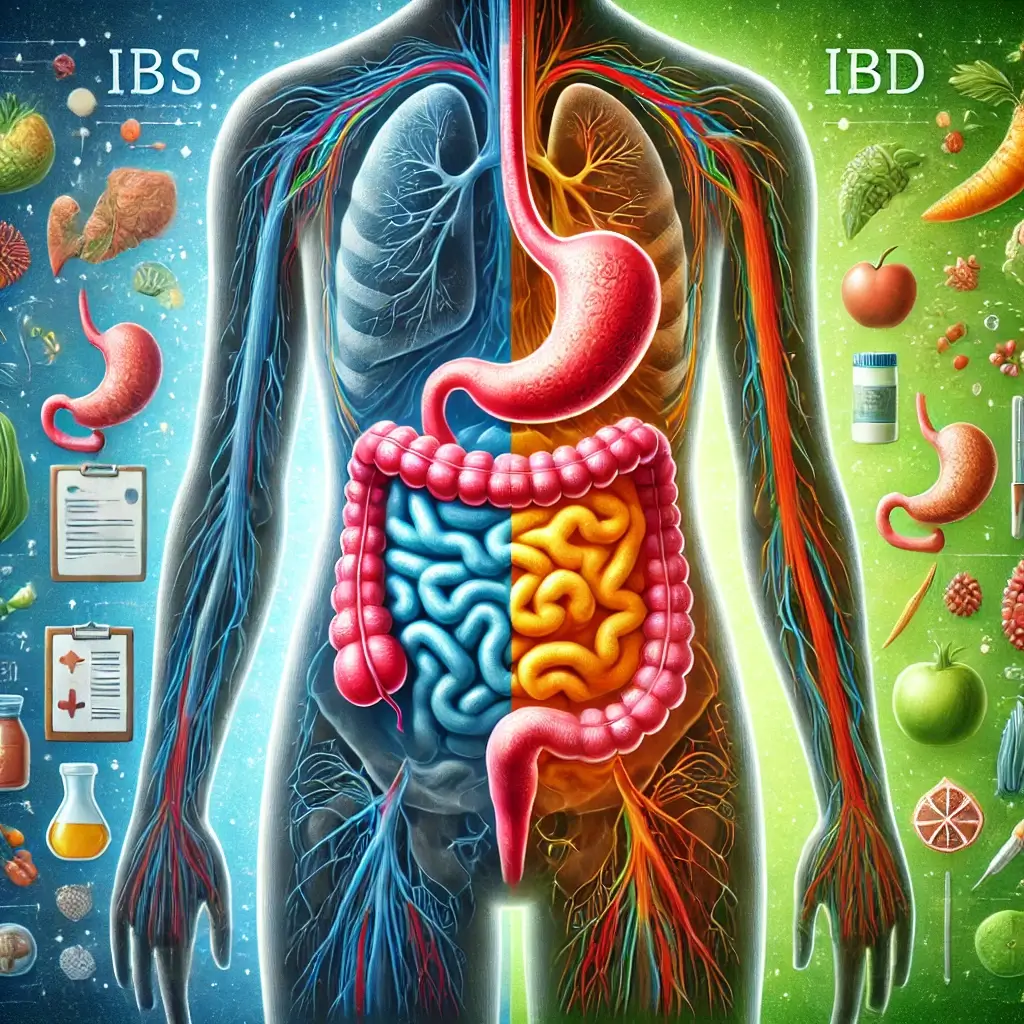
The human digestive system network is a complex network responsible for processing nutrients and expelling waste. When it falters, the results can significantly disrupt daily life. Among the most prevalent digestive conditions are Irritable Bowel Syndrome (IBS) and Inflammatory Bowel Disease (IBD). Despite their similar acronyms and overlapping symptoms, these two disorders are fundamentally distinct in their causes, progression, and management strategies. Misunderstanding these differences can lead to misdiagnosis, delayed treatment, and suboptimal care.
Distinguishing IBS and IBD
IBS is a functional gastrointestinal disorder, meaning it affects how the gut works but does not cause visible damage. It is characterized by chronic abdominal pain, bloating, and altered bowel habits without inflammation or structural abnormalities. In contrast, IBD is an umbrella term for autoimmune diseases, including Crohn’s disease and ulcerative colitis, which cause chronic inflammation and damage to the gastrointestinal tract.
Importance of Understanding Differences
Understanding these distinctions is essential for patients and clinicians alike. This article explores the underlying mechanisms, symptoms, diagnostic approaches, and treatment options for IBS and IBD, highlighting recent medical research and advancements to offer a comprehensive perspective.
Key Differences Between IBS and IBD
1. Underlying Causes
IBS Causes and Mechanisms
IBS: The precise cause of IBS remains elusive, but research suggests a combination of gut motility issues, hypersensitivity to pain, and disruptions in the gut-brain axis. Psychological factors, such as stress and anxiety, often exacerbate symptoms. Recent studies have also implicated alterations in gut microbiota and low-grade inflammation in some IBS cases.
IBD Causes and Mechanisms
IBD: IBD is an autoimmune condition where the immune system mistakenly attacks the gastrointestinal lining. Genetic predisposition and environmental triggers, such as diet and infections, play significant roles. Crohn’s disease can affect any part of the digestive tract, while ulcerative colitis is limited to the colon and rectum. Emerging research suggests that an imbalance in the gut microbiome may drive inflammation in IBD patients.
Symptom Comparison
While both IBS and IBD cause abdominal discomfort and bowel irregularities, their presentations differ significantly in severity and characteristics:
IBS Symptom Profile
IBS Symptoms: Symptoms often include bloating, gas, and alternating diarrhea or constipation. Pain typically improves after a bowel movement, and there’s no rectal bleeding. Stress or certain foods are common triggers for symptom flare-ups.
IBD Symptom Profile
IBD Symptoms: IBD symptoms are more severe and include persistent pain, chronic diarrhea, fatigue, weight loss, and blood in the stool. Unlike IBS, IBD can lead to complications such as strictures, fistulas, and an increased risk of colorectal cancer.
Diagnostic Approaches for IBS
IBS Diagnosis: IBS is diagnosed primarily through a process of exclusion. Physicians use criteria like the Rome IV diagnostic guidelines to identify the condition, ruling out other diseases through comprehensive stool tests, blood work, and imaging studies.
Diagnostic Approaches for IBD
IBD Diagnosis: IBD requires more invasive diagnostic techniques, such as colonoscopy with biopsies and advanced imaging tests. These tests help assess inflammation levels and identify potential complications.
Treatment Strategies for IBS
IBS Treatment: Since IBS has no cure, treatment focuses on comprehensive symptom management. Dietary interventions like the low-FODMAP diet and fiber supplements are commonly recommended. Psychological therapies, including cognitive-behavioral therapy, and medications targeting specific symptoms are also effective.
Treatment Strategies for IBD
IBD Treatment: Treatment for IBD aims to reduce inflammation, manage symptoms, and maintain long-term remission. Options include anti-inflammatory drugs, immune suppressants, and advanced biologics targeting specific inflammatory pathways. In severe cases, surgery may be necessary to remove damaged portions of the bowel.
Latest Research and Medical Advances
Recent studies emphasize the importance of gut microbiome in both IBS and IBD pathogenesis. For IBS, probiotics and fecal microbiota transplants are being investigated as potential therapies. In IBD, advancements in biologic therapies, such as anti-TNF agents and JAK inhibitors, have revolutionized treatment approaches.
Dietary Interventions and Research
Additionally, researchers are exploring the role of specialized diets in managing both conditions. While a low-FODMAP diet shows significant effectiveness for IBS management, specific dietary interventions like exclusive enteral nutrition show promise in managing IBD, particularly in pediatric patients.
Final Insights and Recommendations
IBS and IBD, while sharing some symptoms, are fundamentally different in their underlying causes, severity, and management approaches. IBS affects gut function without causing structural damage, whereas IBD involves chronic inflammation and potential long-term complications. Understanding these distinctions empowers patients to seek timely and appropriate medical care.
Seeking Medical Guidance
If you’re experiencing persistent digestive issues or chronic gastrointestinal symptoms, consult a healthcare provider for an accurate diagnosis and personalized treatment plan. With proper management and ongoing medical support, individuals can effectively navigate their digestive health challenges.
References
Longstreth, J. F., et al. (2016). Functional Gastrointestinal Disorders: Fourth Rome Criteria. Gastroenterology, 150(6), 1392–1402. PMC.
Loftus, E. V., et al. (2017). Clinical Practice Guidelines for Inflammatory Bowel Disease in Adults. Gastroenterology, 152(6), 1471–1500. PMC.
Pittayanon, R., et al. (2019). Gut Microbiota in Patients With Irritable Bowel Syndrome—A Systematic Review. Gastroenterology, 157(1), 97–108.
Ni, J., et al. (2017). Gut Microbiota and IBD: Causation or Correlation? Nature Reviews Gastroenterology & Hepatology, 14(10), 573–584.
Mullish, B. H., et al. (2020). The Use of Faecal Microbiota Transplant as Treatment for Recurrent or Severe Clostridium difficile Infection and Other Potential Indications. Journal of Internal Medicine, 288(6), 678–694.
Feuerstein, J. D., et al. (2020). Systematic Review and Meta-Analysis of Anti-TNF Therapy for Inflammatory Bowel Disease. Alimentary Pharmacology & Therapeutics, 51(8), 740–751.
Sigall-Boneh, R., et al. (2017). Dietary Therapy With the Crohn’s Disease Exclusion Diet Is a Successful Strategy for Induction of Remission in Children and Young Adults Failing Biological Therapy. Journal of Crohn’s and Colitis, 11(10), 1205–1212.