Introduction to Antibiotics and Gut Health
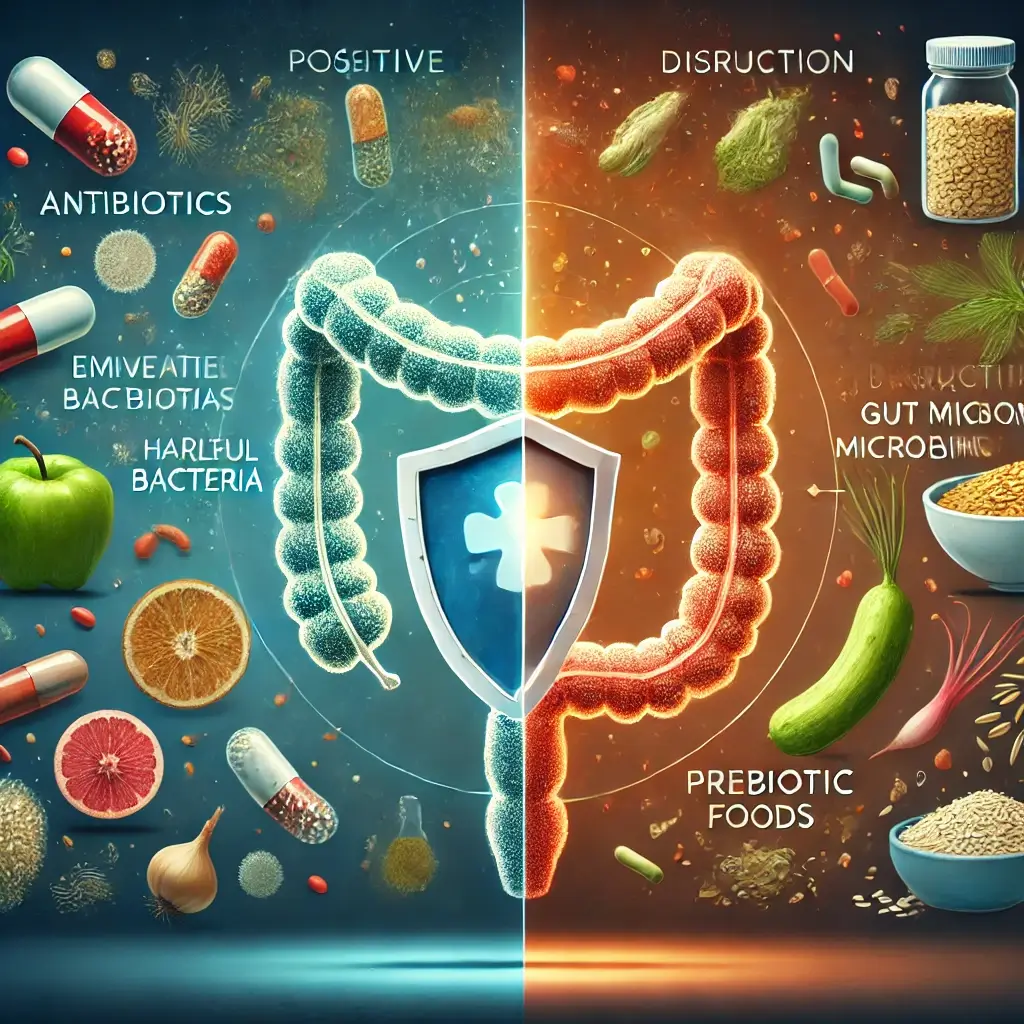
Antibiotics revolutionizing modern medicine have transformed healthcare, offering an effective defense against bacterial infections that were once life-threatening. These medications work by targeting and eliminating harmful bacteria, but their mechanism of action is not selective. Antibiotics disrupting beneficial gut bacteria often impact the delicate balance of beneficial bacteria residing in the gut microbiome—a vast, intricate ecosystem of microorganisms crucial for digestion, immune health, and overall well-being.
This unintended consequence can lead to a host of digestive issues, including diarrhea, bloating, and antibiotic-associated colitis. Beyond immediate symptoms, long-term disruptions in gut health have been linked to weakened immune function and a higher risk of metabolic and autoimmune disorders. Understanding the interplay between antibiotics and gut health is essential for mitigating these effects and ensuring a swift recovery of the microbiome.
The Science of Antibiotic-Induced Gut Disruptions
Antibiotics are essential for managing bacterial infections, but their broad-spectrum nature can disrupt the gut microbiome in several ways:
Impact on Microbial Diversity
Antibiotics reducing microbial diversity diminish the population of beneficial species while inadvertently allowing opportunistic pathogens to thrive. For instance, a depletion of protective bacteria can lead to an overgrowth of Clostridioides difficile (C. diff), a dangerous pathogen that causes severe diarrhea and inflammation.
Metabolic Function Changes
Beneficial gut bacteria metabolizing nutrients play a role in metabolizing nutrients and producing short-chain fatty acids (SCFAs), which are vital for colon health. Antibiotic-induced metabolic imbalances can disrupt these processes, leading to gastrointestinal symptoms such as bloating and gas.
Impact on Immune Defense
The gut microbiome is a critical component of the immune system. Antibiotic-induced immune system disruptions can impair the gut’s ability to fend off pathogens, leaving the body vulnerable to recurring infections.
Recent Medical Research Findings
A 2023 study in Nature Medicine investigated the long-term impact of antibiotics on gut microbiota. Researchers found that even a single course of antibiotics could significantly reduce microbial diversity for months. This highlights the need for effective interventions to restore gut health and prevent lasting damage.
Probiotic Solutions
A 2022 review published in Gastroenterology examined the role of probiotics in preventing antibiotic-associated diarrhea. The study concluded that specific strains, such as Lactobacillus and Bifidobacterium, effectively reduced symptoms and expedited the recovery of beneficial gut bacteria.
Dietary Influence on Gut Recovery
Another study in Current Opinion in Clinical Nutrition found that diets enhancing gut microbiota resilience post-antibiotic treatment showed promising results. Foods like oats, bananas, and asparagus were particularly effective in fueling the regrowth of beneficial bacteria.
Practical Steps for Gut Recovery
Incorporating high-quality probiotic supplements can help replenish beneficial bacteria. Look for multi-strain products containing Lactobacillus acidophilus and Bifidobacterium bifidum. Natural probiotic food sources like yogurt, kefir, sauerkraut, and kimchi can help rebuild microbial diversity.
The Role of Prebiotics
Prebiotic-rich foods supporting gut bacteria, found in foods like garlic, onions, and whole grains, serve as food for beneficial bacteria, promoting their growth. Sufficient hydration supports digestion and nutrient absorption.
Conclusion and Future Implications
As scientific research continues to uncover the complexities of gut microbiome restoration, adopting evidence-based strategies for gut restoration ensures that the benefits of antibiotics are maximized while minimizing their unintended consequences. If symptoms persist beyond antibiotic treatment, consulting a healthcare provider is essential for personalized guidance.
References
Blaser, M. J., McDonough, M. H., & Ugalde, J. A. (2023). Post-antibiotic gut microbiome restoration: Challenges and opportunities. Nature Medicine, 29(1), 18–30.
Goldenberg, J. Z., Lyons, A., Gibson, G. R., Huttenhower, C., & Dewitt, T. C. (2022). Probiotics for antibiotic-associated diarrhea prevention in adults and children. Gastroenterology, 162(7).
Gibson, G. R., Huttenhower, C., & Scott, K. P. (2022). Prebiotics and gut microbiome mechanisms: Mechanisms and benefits. Current Opinion in Clinical Nutrition & Metabolic Care, 25(3), 215–220.