The Foundation of Digestive Health
Digestive health is a cornerstone of overall well-being, influencing not just physical comfort but also mental health, energy levels, and productivity. For millions of individuals living with chronic digestive disorders such as Irritable Bowel Syndrome (IBS) or other functional gastrointestinal disorders (FGIDs), daily life can feel like navigating a minefield of triggers. Symptoms such as bloating, abdominal pain, excessive gas, and unpredictable bowel movements often interfere with both personal and professional activities.
The Science-Driven Dietary Approach
In response to these challenges, the Low-FODMAP diet has emerged as a science-driven dietary approach. Developed by researchers at Monash University, this diet is based on the principle of identifying and managing food sensitivities to alleviate symptoms. Unlike fad diets that promise generic benefits, the Low-FODMAP diet is evidence-based and highly personalized, providing targeted relief for those suffering from gastrointestinal discomfort.
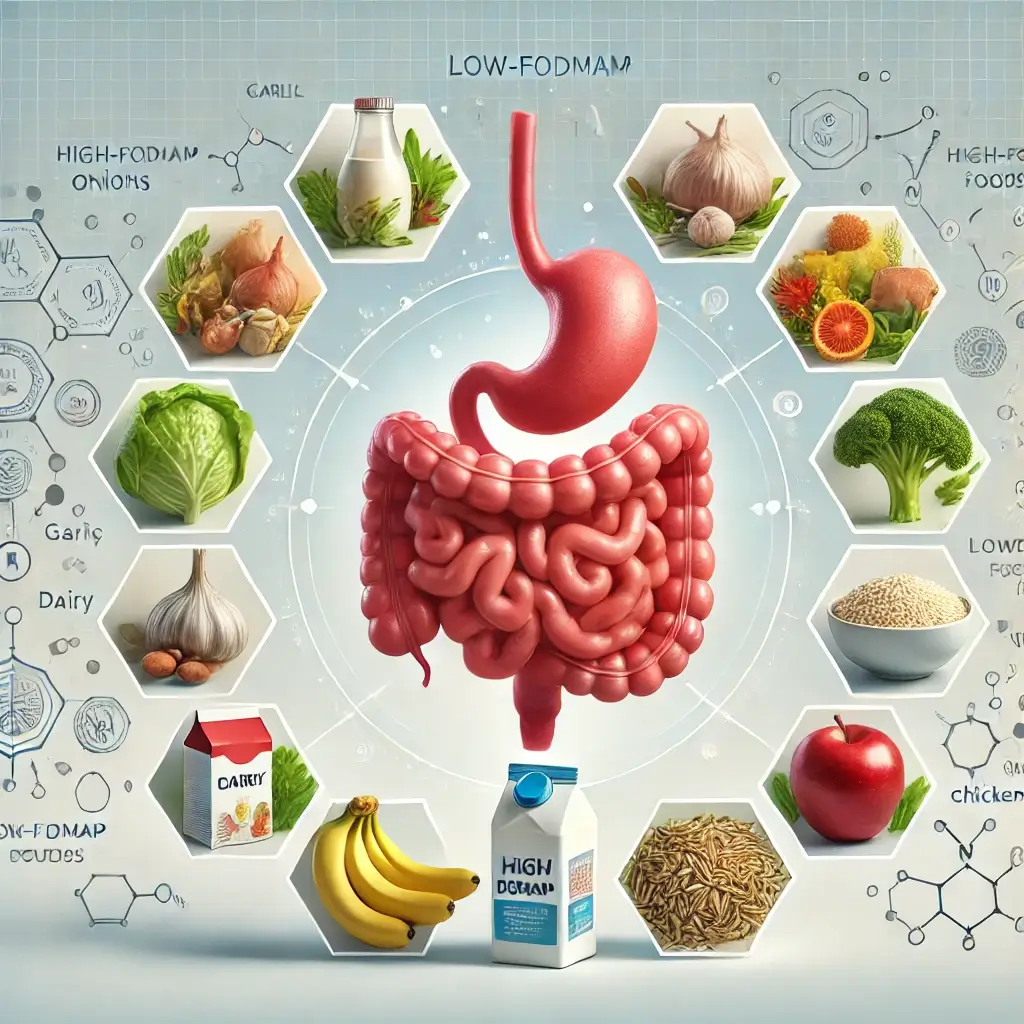
Understanding FODMAPs: Digestive Triggers Unveiled
FODMAPs—short for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols—are a group of poorly absorbed short-chain carbohydrates. Found in various foods such as dairy, wheat, legumes, and certain fruits, FODMAPs are known to cause digestive symptoms in sensitive individuals. When these compounds reach the large intestine, they ferment, producing gases like hydrogen and methane. This fermentation can lead to distension, pain, and altered bowel habits in susceptible people (Gibson & Shepherd, 2010).
FODMAP Categories
The goal of the Low-FODMAP diet is to identify specific FODMAP subgroups that exacerbate symptoms. This dietary approach categorizes FODMAPs into four main types:
- Oligosaccharides: Found in wheat, onions, and garlic.
- Disaccharides: Primarily lactose in dairy products.
- Monosaccharides: Found in fructose-heavy fruits and sweeteners.
- Polyols: Sugar alcohols like sorbitol and mannitol, common in artificial sweeteners and certain fruits.
Medical Evidence and Research Support
The effectiveness of the Low-FODMAP diet is backed by robust research. A systematic review published in Nutrients (2017) examined 22 clinical studies on IBS patients, concluding that the diet significantly reduced bloating, abdominal pain, and irregular stool patterns compared to standard dietary advice. Researchers noted improved quality of life in participants, reinforcing the diet’s value for IBS management (Ong et al., 2017).
Beyond IBS: Additional Applications
Further research has demonstrated the diet’s versatility beyond IBS. A 2018 study in Alimentary Pharmacology & Therapeutics highlighted its efficacy in managing FGIDs, showcasing reductions in symptoms such as abdominal pain and diarrhea in patients without IBS diagnoses. This finding underscores the potential for broader applications in gut health (Staudacher et al., 2018).
Individual Response Variability
However, the diet is not a universal solution. A study published in Clinical Gastroenterology and Hepatology in 2020 found variability in patient responses, with some participants experiencing limited or no relief. These findings highlight the importance of tailoring the diet to individual needs and the necessity for professional guidance during the process (Halmos et al., 2020).
The Three-Phase Approach
Elimination Phase: Lasting 4-6 weeks, this phase requires strict removal of all high-FODMAP foods to establish a baseline of symptom control.
Reintroduction Phase: Specific FODMAP groups are reintroduced one at a time, allowing individuals to identify personal triggers.
Maintenance Phase: With triggers identified, patients adopt a long-term diet that minimizes high-FODMAP foods while maintaining nutritional variety.
Essential Resources
Monash University FODMAP App: This app provides comprehensive food databases and portion guides.
Professional Guidance: Consulting a dietitian ensures nutritional adequacy and proper adherence.
Community and Recipes: Online forums and cookbooks offer support and inspiration for meal planning.
Final Insights
The Low-FODMAP diet is a scientifically validated method for managing chronic digestive issues, offering tailored relief to those affected by IBS and other FGIDs. While not a one-size-fits-all solution, it provides a structured framework for identifying dietary triggers and improving quality of life. Patients considering this diet should work closely with healthcare professionals to maximize its benefits and ensure long-term success.
References
Gibson, P. R., & Shepherd, S. J. (2010). Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. Journal of Gastroenterology and Hepatology, 25(2), 252-258.
Ong, D. K., et al. (2017). The Low-FODMAP diet improves symptoms of irritable bowel syndrome: A systematic review and meta-analysis. Nutrients, 9(9), 940.
Staudacher, H. M., et al. (2018). Mechanisms and efficacy of dietary FODMAP restriction in IBS. Alimentary Pharmacology & Therapeutics, 47(6), 702-720.
Halmos, E. P., et al. (2020). A randomised-controlled trial of a Low-FODMAP diet for IBS. Clinical Gastroenterology and Hepatology, 18(6), 131-141.